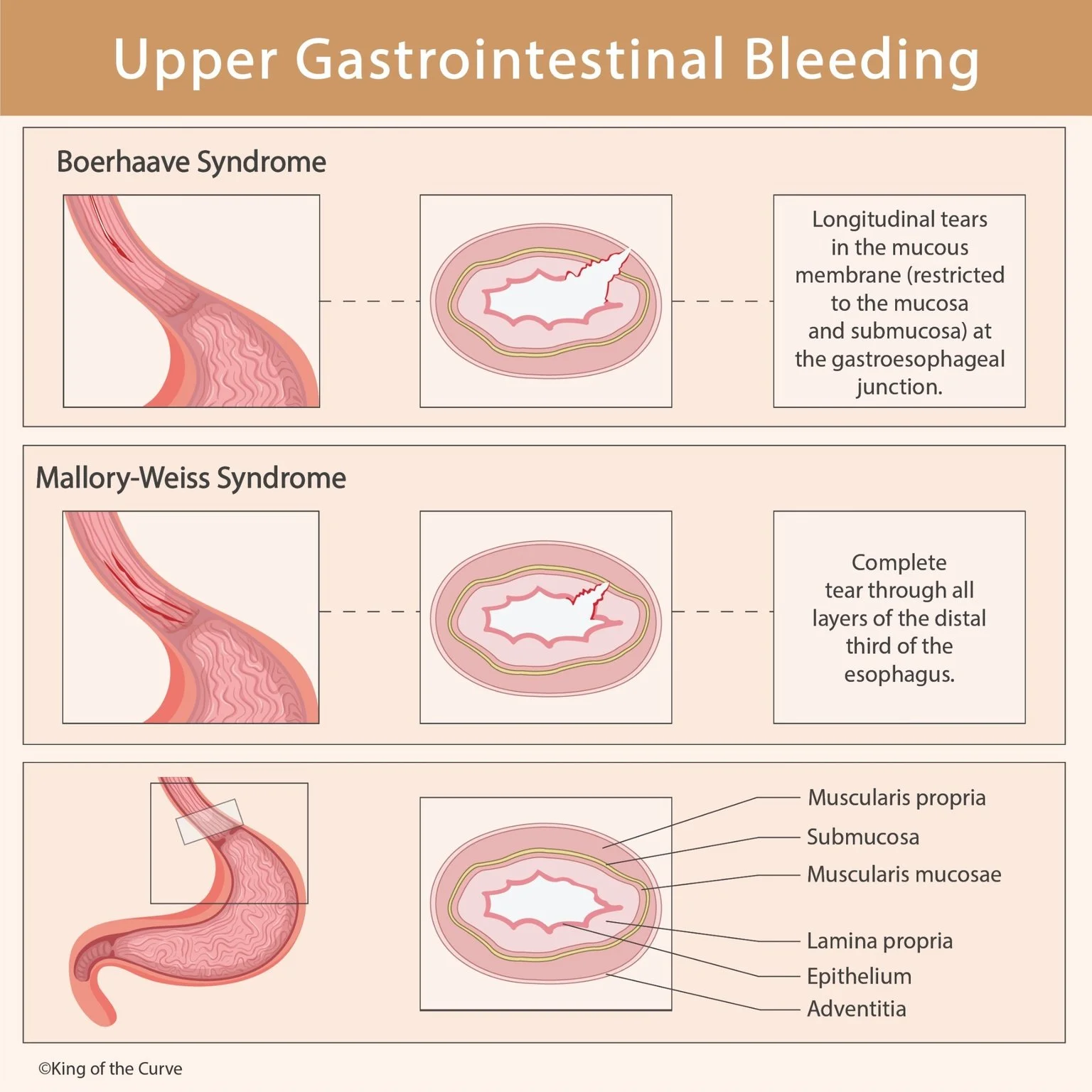
Upper Gastrointestinal Bleeding: Boerhaave vs Mallory-Weiss Syndrome
Upper gastrointestinal (GI) bleeding is a common and sometimes life-threatening medical condition that often presents with hematemesis (vomiting blood) or melena (black tarry stools). Among its causes, Boerhaave syndrome and Mallory Weiss syndrome are two important conditions that result from esophageal injury, usually after episodes of forceful vomiting.
✅ What Happens During Vomiting?
When a person vomits forcefully, the pressure inside the stomach and esophagus rises sharply. If that pressure becomes excessive, it may lead to tearing of the esophageal lining.
This injury can range from:
superficial mucosal tears (Mallory-Weiss)
tofull-thickness rupture (Boerhaave)
Mallory-Weiss Syndrome
📌 Definition
Mallory-Weiss syndrome is caused by longitudinal mucosal tears at the gastroesophageal junction, typically after repeated vomiting or retching.
🧠 Key Mechanism
✔ Partial tear
✔ Limited to the mucosa and submucosa
✔ Usually not life-threatening, but can cause bleeding
Common Triggers
Excessive alcohol use
Eating disorders (bulimia)
Severe coughing
Pregnancy-related vomiting
Seizure-related vomiting
Clinical Presentation
Painful hematemesis after vomiting
Bright red or coffee-ground blood
Mild epigastric discomfort
Treatment
Most cases resolve without intervention, but if bleeding persists:
✅ IV fluids
✅ Proton pump inhibitors (PPIs)
✅ Endoscopic hemostasis (clipping, cautery)
✅ Rarely requires surgery
Boerhaave Syndrome
📌 Definition
Boerhaave syndrome is a spontaneous full-thickness rupture of the esophagus caused by sudden increase in intraesophageal pressure—most often due to forceful vomiting.
🧠 Key Mechanism
❗ Complete tear through all layers
❗ Leads to leakage of esophageal contents into the mediastinum
❗ Causes mediastinitis, sepsis, and shock if untreated
Classic Trigger
Forceful vomiting after heavy meals or alcohol
Clinical Presentation
This is a medical emergency. Typical findings include:
Severe chest pain after vomiting
Subcutaneous emphysema (air under skin)
Tachycardia, fever
Dyspnea (difficulty breathing)
Signs of septic shock in severe cases
✨ Classic Triad (Mackler triad):
Vomiting
Chest pain
Subcutaneous emphysema
Treatment
✅ Immediate stabilization
✅ Broad-spectrum antibiotics
✅ CT esophagography (diagnosis)
✅ Surgical repair or endoscopic stenting
✅ ICU monitoring
📊 Comparison Table: Boerhaave vs Mallory-Weiss
| Feature | Mallory-Weiss Syndrome | Boerhaave Syndrome |
|---|---|---|
| Depth of tear | Mucosa / submucosa only | Full-thickness rupture |
| Location | Gastroesophageal junction | Distal esophagus |
| Main problem | Bleeding | Perforation + mediastinitis |
| Symptoms | Hematemesis, mild pain | Severe chest pain, sepsis |
| Severity | Often self-limited | Life-threatening emergency |
| Treatment | Supportive ± endoscopy | Surgery + antibiotics |
Key Takeaway
✅ Mallory-Weiss = mucosal tear → bleeding
🚨 Boerhaave = full rupture → infection + sepsis
If a patient has vomiting followed by chest pain and systemic toxicity, always think Boerhaave syndrome and act fast.
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.