🧠 Gastrointestinal Secretory Cells: An Integrated Overview
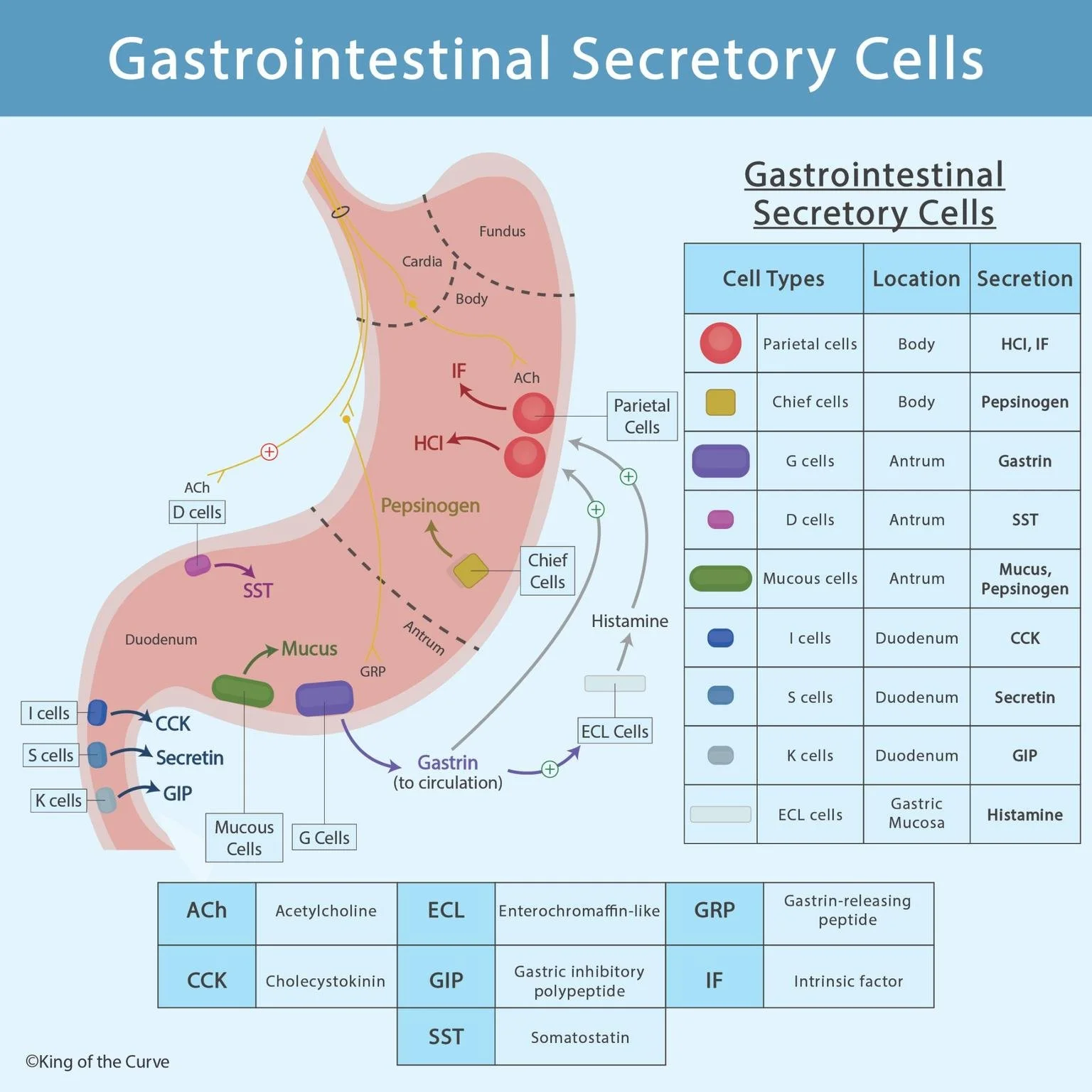
The gastrointestinal (GI) tract relies on a highly coordinated network of specialized secretory cells to regulate digestion, absorption, and protection of the mucosa. These cells are distributed across the stomach and duodenum and communicate through neural, hormonal, and paracrine signaling pathways. The diagram illustrates how these cells interact to finely control gastric acid secretion, enzyme release, and intestinal function.
🔬 Parietal and Chief Cells: Acid and Enzyme Production
Parietal cells, located primarily in the body and fundus of the stomach, secrete hydrochloric acid (HCl) and intrinsic factor (IF). HCl creates an acidic environment necessary for protein digestion and activation of enzymes, while intrinsic factor is essential for vitamin B₁₂ absorption in the terminal ileum. Parietal cells are stimulated by acetylcholine (ACh), gastrin, and histamine, with histamine acting via a powerful paracrine mechanism.
Chief cells, also found in the gastric body, release pepsinogen, the inactive precursor of pepsin. Once exposed to gastric acid, pepsinogen is converted to pepsin, initiating protein digestion.
🧪 G Cells and D Cells: Hormonal Balance in the Antrum
G cells, located in the gastric antrum, secrete gastrin in response to vagal stimulation (via GRP) and the presence of peptides in the stomach. Gastrin enters systemic circulation and stimulates parietal cells directly and indirectly by activating enterochromaffin-like (ECL) cells to release histamine.
In contrast, D cells produce somatostatin (SST), a potent inhibitory hormone that suppresses gastrin release and gastric acid secretion. This negative feedback mechanism protects the stomach from excessive acidity and mucosal injury.
🧬 Enterochromaffin-Like (ECL) Cells: Paracrine Amplifiers
ECL cells, located in the gastric mucosa, secrete histamine in response to gastrin and ACh. Histamine binds to H₂ receptors on parietal cells, significantly amplifying acid secretion. This paracrine interaction represents one of the most important regulatory steps in gastric physiology.
🧃 Mucous Cells: Gastric Protection
Mucous cells, found mainly in the antrum, secrete mucus and bicarbonate, forming a protective barrier that shields the gastric epithelium from acid and enzymatic damage. This defense mechanism is critical for maintaining mucosal integrity.
🧠 Duodenal Enteroendocrine Cells: Coordinating Digestion
Several specialized endocrine cells reside in the duodenum and regulate downstream digestive processes:
I cells secrete cholecystokinin (CCK), which stimulates pancreatic enzyme secretion and gallbladder contraction.
S cells release secretin, promoting bicarbonate secretion from the pancreas to neutralize gastric acid.
K cells produce GIP (gastric inhibitory peptide), which reduces gastric acid secretion and enhances insulin release after meals.
These hormones ensure smooth coordination between the stomach, pancreas, liver, and intestines.
📊 Gastrointestinal Secretory Cells – Summary Table
| Cell Type | Primary Location | Major Secretion(s) | Main Function |
|---|---|---|---|
| Parietal cells | BodyFundus | HClIntrinsic factor (IF) | Acid secretion for digestion; IF for vitamin B12 absorption |
| Chief cells | Body | Pepsinogen | Protein digestion (converted to pepsin in acidic pH) |
| G cells | Antrum | Gastrin | Stimulates acid secretion (directly and via ECL cells) |
| D cells | Antrum | Somatostatin (SST) | Inhibits gastrin and gastric acid secretion |
| ECL cells | Gastric mucosa | Histamine | Paracrine stimulation of parietal cells (H2 receptors) |
| Mucous cells | Antrum | MucusBicarbonate | Protects gastric mucosa from acid injury |
| I cells | Duodenum | CCK | Stimulates pancreatic enzymes & gallbladder contraction |
| S cells | Duodenum | Secretin | Stimulates pancreatic bicarbonate secretion |
| K cells | Duodenum | GIP | Decreases gastric acid; increases insulin release |
🔁 Neural and Hormonal Integration
The diagram highlights the interaction between vagal (parasympathetic) stimulation, local hormones, and paracrine mediators. Acetylcholine directly stimulates parietal and chief cells, while gastrin and histamine reinforce acid production. Inhibitory signals such as somatostatin ensure balance, preventing pathological hypersecretion.
📌 Clinical Relevance
Understanding gastrointestinal secretory cells is essential for interpreting conditions such as:
Peptic ulcer disease
Zollinger–Ellison syndrome
Pernicious anemia
Pharmacologic actions of H₂ blockers and proton pump inhibitors
The integrated signaling shown in this diagram explains why multiple therapeutic targets exist in acid-related disorders.
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.