🩺 Anatomy of Inguinal and Femoral Hernia: A Clinical Overview
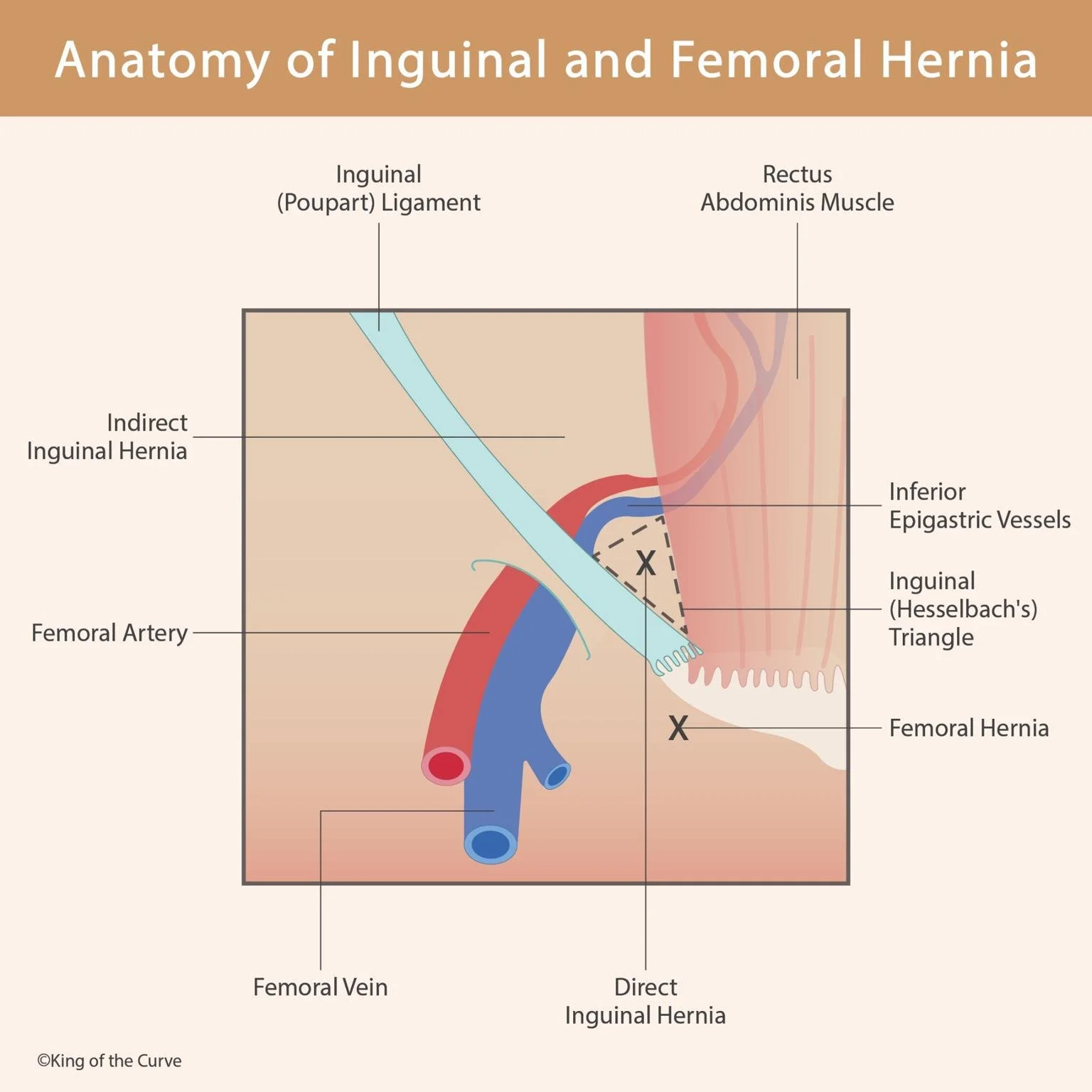
Hernias are common conditions in both clinical practice and surgical settings. Among them, inguinal and femoral hernias are the most frequent types seen in the lower abdominal region. This blog post explores the anatomy, location, and clinical significance of these hernias using the labeled visual guide provided above.
📌 What is a Hernia?
A hernia occurs when a part of an organ or tissue protrudes through a weak spot in the surrounding muscles or connective tissue. In the inguinal and femoral regions, hernias occur when abdominal contents, such as intestinal loops, push through the abdominal wall near the groin.
🧠 Understanding the Key Structures
The diagram outlines important anatomical landmarks involved in inguinal and femoral hernias:
1. Inguinal (Poupart’s) Ligament
A fibrous band running from the pubic tubercle to the anterior superior iliac spine (ASIS).
Forms the base of the inguinal canal, a common site for hernias.
2. Inferior Epigastric Vessels
These vessels serve as a critical landmark to differentiate between direct and indirect inguinal hernias:
Hernias lateral to these vessels = Indirect
Hernias medial to these vessels = Direct
3. Hesselbach’s Triangle (Inguinal Triangle)
Defined by:
Medial border: Lateral edge of the rectus abdominis
Lateral border: Inferior epigastric vessels
Inferior border: Inguinal ligament
Direct inguinal hernias protrude through this triangle.
4. Rectus Abdominis Muscle
Forms the medial wall of Hesselbach’s triangle and contributes to the abdominal wall's integrity.
🔍 Types of Hernias Illustrated
➤ Indirect Inguinal Hernia
Passes through the deep inguinal ring, lateral to the inferior epigastric vessels.
Common in younger males due to a persistent processus vaginalis.
May descend into the scrotum.
➤ Direct Inguinal Hernia
Protrudes medially to the inferior epigastric vessels within Hesselbach’s triangle.
Common in older adults due to weakening abdominal muscles.
Rarely descends into the scrotum.
➤ Femoral Hernia
Passes below the inguinal ligament through the femoral canal.
More common in females, due to a wider pelvic structure.
High risk of incarceration and strangulation due to tight femoral ring.
🔬 Clinical Significance
Diagnosis: Based on physical exam, sometimes confirmed by imaging (e.g., ultrasound or CT).
Complications: Bowel obstruction, incarceration, and strangulation.
Treatment: Surgical repair (open or laparoscopic) is often required to prevent complications.
📝 Summary Table
| Hernia Type | Location | Common Demographic | Risk Level |
|---|---|---|---|
| Indirect Inguinal | Lateral to inferior epigastric vessels | Young males | Moderate |
| Direct Inguinal | Medial to inferior epigastric vessels | Older adults | Moderate |
| Femoral | Below inguinal ligament | Females | High |
📚 Final Thoughts
A solid understanding of the anatomy of the inguinal region is critical for diagnosing and managing hernias effectively. This diagram not only illustrates the spatial relationships of each hernia type but also highlights the key landmarks that guide surgical intervention.
Whether you’re a medical student, healthcare professional, or curious learner, grasping these basics is essential for interpreting clinical scenarios involving groin hernias.
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.