🔎 Enteropathic Arthritis: Causes, Symptoms, and Associations
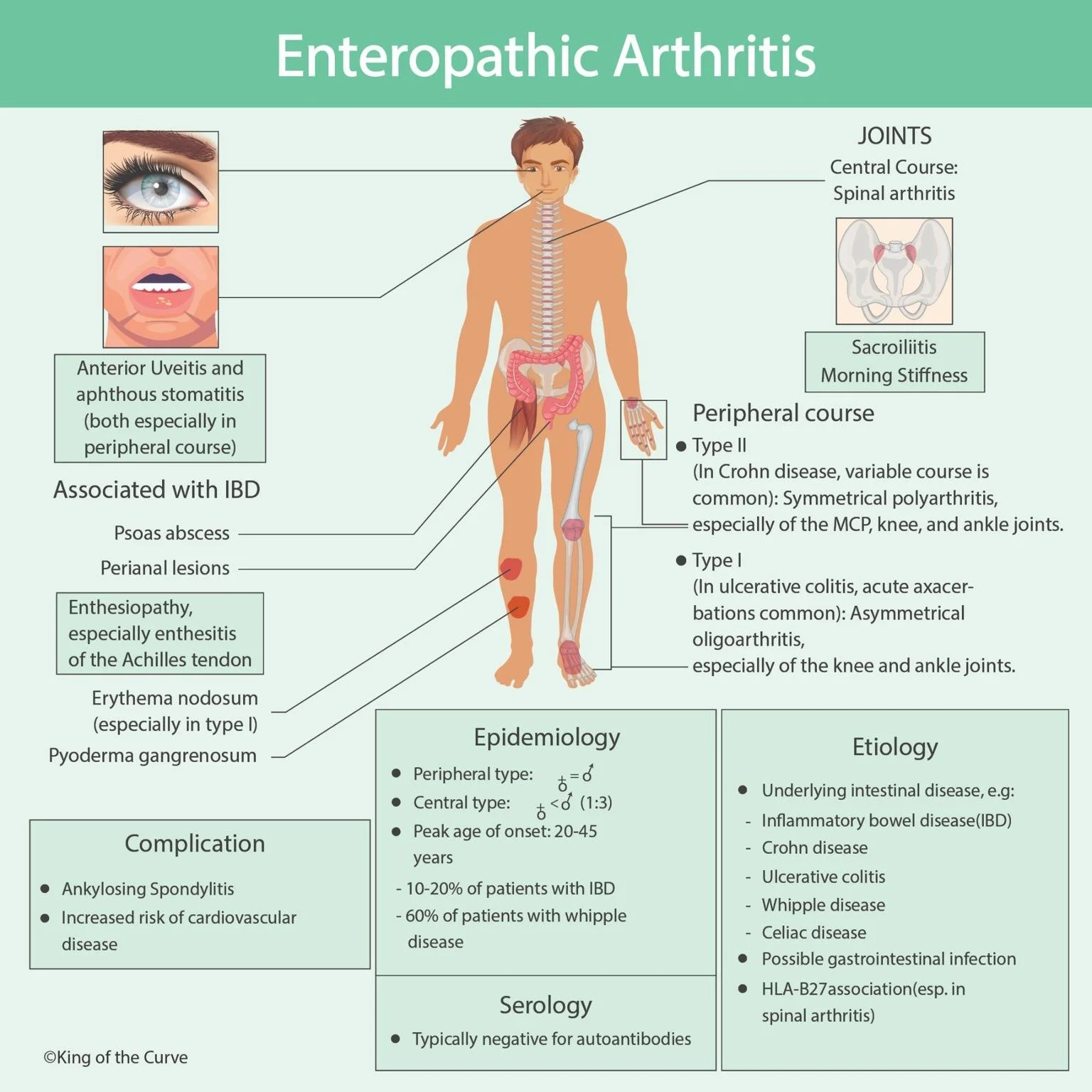
Enteropathic Arthritis (EA) is a type of inflammatory arthritis strongly associated with chronic intestinal diseases, particularly inflammatory bowel disease (IBD) such as Crohn’s disease and ulcerative colitis. It presents as a spectrum of symptoms affecting not only the joints but also the eyes, skin, and other organ systems, making it a systemic condition that requires careful management.
🔎 What is Enteropathic Arthritis?
Enteropathic arthritis is an extraintestinal manifestation of IBD. It can present in two major forms:
Central course: Spinal arthritis (spondyloarthritis) and sacroiliitis, often leading to morning stiffness.
Peripheral course:
Type I: Asymmetrical oligoarthritis, commonly affecting large joints such as the knees and ankles.
Type II: Symmetrical polyarthritis, affecting smaller joints like MCP (metacarpophalangeal), knee, and ankle joints.
👁️ Extra-Articular Features
Beyond joint pain and stiffness, patients often experience:
Eye involvement: Anterior uveitis.
Oral lesions: Aphthous stomatitis.
Skin manifestations: Erythema nodosum, pyoderma gangrenosum.
Tendon involvement: Enthesopathy, especially Achilles tendon enthesitis.
Perianal lesions and psoas abscesses (in Crohn’s disease).
📊 Epidemiology
| Epidemiology of Enteropathic Arthritis |
|---|
| Peripheral arthritis is more common in men |
| Central type arthritis has a male predominance (1:3) |
| Peak onset occurs between 20–45 years |
| Occurs in 10–20% of patients with IBD |
| Seen in up to 60% of patients with Whipple disease |
🧬 Etiology and Pathogenesis
Enteropathic arthritis arises due to the interaction of genetic, immune, and environmental factors.
Triggered by underlying intestinal disease such as Crohn’s disease, ulcerative colitis, celiac disease, and Whipple disease.
Possible links with gastrointestinal infections.
Strong association with HLA-B27, especially in spinal arthritis.
⚠️ Complications
Patients with enteropathic arthritis are at risk of developing:
Ankylosing spondylitis, leading to chronic spinal stiffness.
Cardiovascular complications, which can increase morbidity.
🧪 Serology
Unlike other autoimmune arthritides, serological tests are usually negative for autoantibodies, which helps differentiate it from conditions such as rheumatoid arthritis.
✅ Key Takeaway
Enteropathic arthritis highlights the gut-joint connection, showing how chronic intestinal inflammation can extend beyond the digestive tract to affect multiple body systems. Early recognition is crucial for improving quality of life, preventing complications, and tailoring treatments that address both IBD and joint involvement.
🔔 Call to Action:
If you or a loved one experience persistent joint pain, stiffness, or swelling alongside digestive issues, consult a rheumatologist or gastroenterologist. Early diagnosis and management can prevent long-term complications and improve overall well-being.
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.