🩸 Transfusion Reactions Explained: High-Yield Guide for MCAT, NCLEX, and USMLE
Blood transfusion reactions are some of the most testable immune concepts across healthcare exams because they combine immunology, hematology, and clinical reasoning. This topic shows up frequently on the NCLEX (recognize symptoms + nursing intervention), the MCAT (antibody/antigen compatibility and immune pathways), and the USMLE (reaction timing + mechanisms). Today, I’m going to break down every major transfusion reaction in a way that makes it easy to remember—and even easier to answer exam questions quickly.
🧠 Why Transfusion Reactions Happen (The Big Idea)
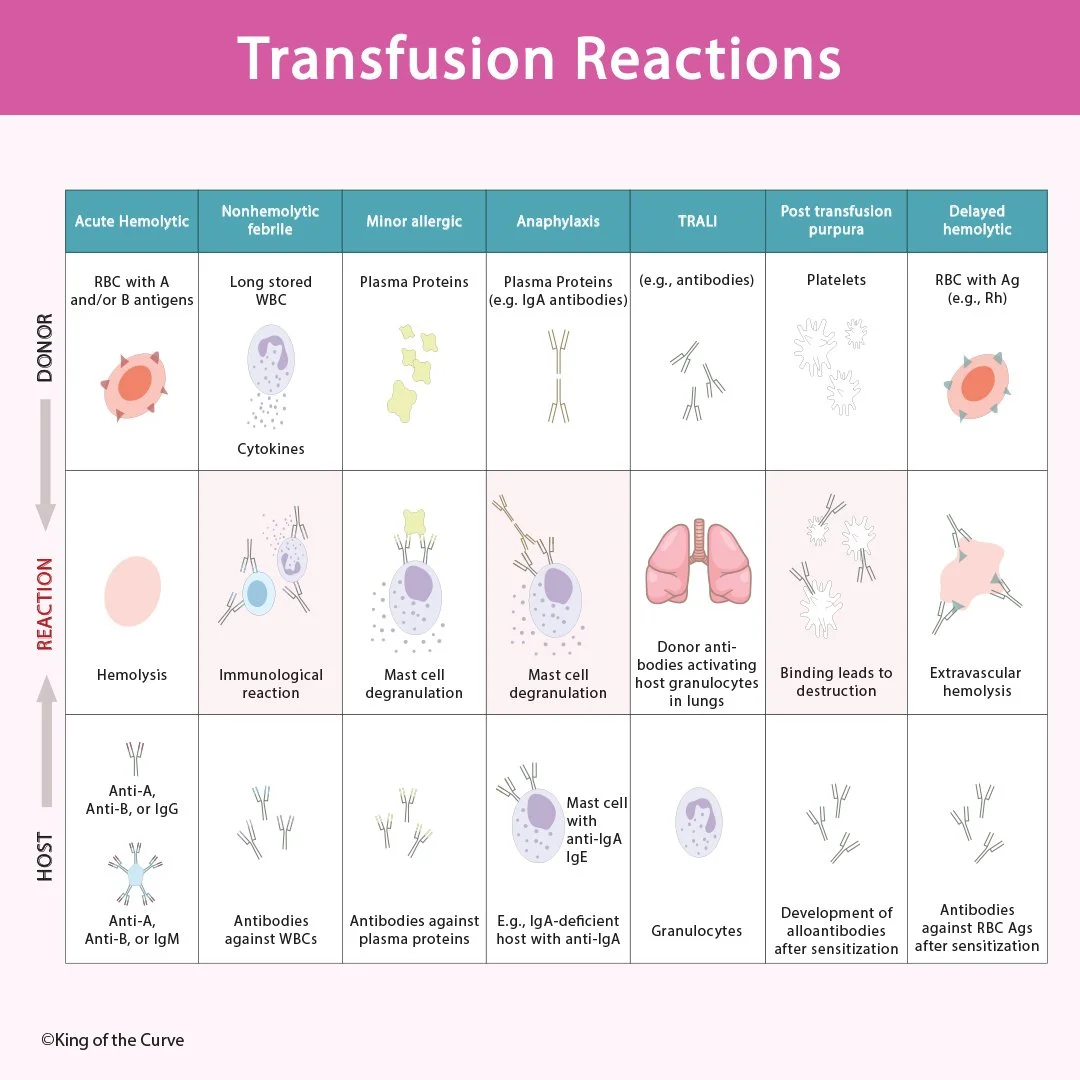
A transfusion reaction happens when the recipient’s immune system identifies something in the donor blood as foreign, triggering antibodies or immune cells. Some reactions come from incompatibility between RBC antigens (like ABO or Rh), while others come from plasma proteins, white blood cell cytokines, or platelet antigens. That’s why it’s not enough to memorize names—you want to understand what part of the donor blood is causing the immune response and what immune mechanism gets activated.
🚨 Acute Hemolytic Transfusion Reaction (Most Dangerous + Most Tested)
This is the classic “wrong blood type” emergency and one of the highest-yield reaction types for all exams. It usually occurs when donor RBCs contain A or B antigens that react with the host’s pre-existing anti-A or anti-B IgM antibodies. This triggers rapid complement activation, causing intravascular hemolysis, fever, hypotension, hemoglobinuria, and can lead to shock. On the NCLEX, this scenario typically tests whether you immediately stop the transfusion, keep the IV line open with saline, and notify the provider.
🌡️ Febrile Nonhemolytic vs Allergic vs Anaphylaxis (The Common Confusion Set)
Febrile nonhemolytic reactions are caused by cytokines and long-stored donor WBCs, leading to fever and chills without hemolysis. These are uncomfortable but not usually life-threatening, and are often prevented with acetaminophen in sensitive patients. Allergic transfusion reactions are driven by sensitivity to plasma proteins, causing hives, itching, and sometimes mild bronchospasm. The severe version is anaphylaxis, which can occur especially in IgA-deficient patients who have anti-IgA antibodies—this leads to airway swelling, wheezing, hypotension, and requires immediate epinephrine.
🫁 TRALI: The Lung Emergency Students Forget (But Exams Love)
TRALI (Transfusion-Related Acute Lung Injury) is tested because it presents like an acute respiratory emergency shortly after transfusion. It occurs when donor antibodies activate host neutrophils in the lungs, causing inflammation, pulmonary edema, and hypoxia. The key detail is timing: TRALI usually develops within 6 hours, and the symptoms look like sudden dyspnea and low oxygen with bilateral infiltrates. On exams, TRALI is often contrasted with volume overload—TRALI is immune-mediated and typically occurs quickly after transfusion.
⏳ Delayed Hemolytic Reaction + Post-Transfusion Purpura (The “Days Later” Reactions)
Delayed hemolytic transfusion reactions happen when a patient was previously sensitized (often via pregnancy or prior transfusion) and later produces IgG antibodies against RBC antigens such as Rh. This leads to extravascular hemolysis, anemia, jaundice, and symptoms that appear days after the transfusion. Post-transfusion purpura is a platelet-mediated reaction where the patient forms antibodies against donor platelets, causing thrombocytopenia and purpura several days later. MCAT and USMLE passages often test the idea that delayed reactions occur after a sensitization step, making timing the biggest clue.
📊 Quick Comparison Table (High-Yield Memory Tool)
| Reaction | Cause | Key Symptom Pattern | High-Yield Exam Clue |
|---|---|---|---|
| Acute Hemolytic | ABO mismatch (IgM → complement) | Fever, hypotension, hemoglobinuria | “Wrong blood type” + shock signs |
| Febrile Nonhemolytic | Cytokines / donor WBCs | Fever + chills only | No hemolysis; improves with acetaminophen |
| Minor Allergic | Plasma proteins | Hives + itching | Mild urticaria after transfusion |
| Anaphylaxis | IgA deficiency + anti-IgA | Airway swelling + hypotension | Wheezing/angioedema + rapid collapse |
| TRALI | Donor antibodies activating neutrophils | Acute respiratory distress | Pulmonary edema within 6 hours |
| Post-transfusion Purpura | Platelet antibodies | Thrombocytopenia + purpura | Platelet destruction days later |
| Delayed Hemolytic | Anti-Rh/other IgG | Anemia + jaundice days later | Extravascular hemolysis after sensitization |
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.