🧠 Mechanism of Immune Complex Deposition
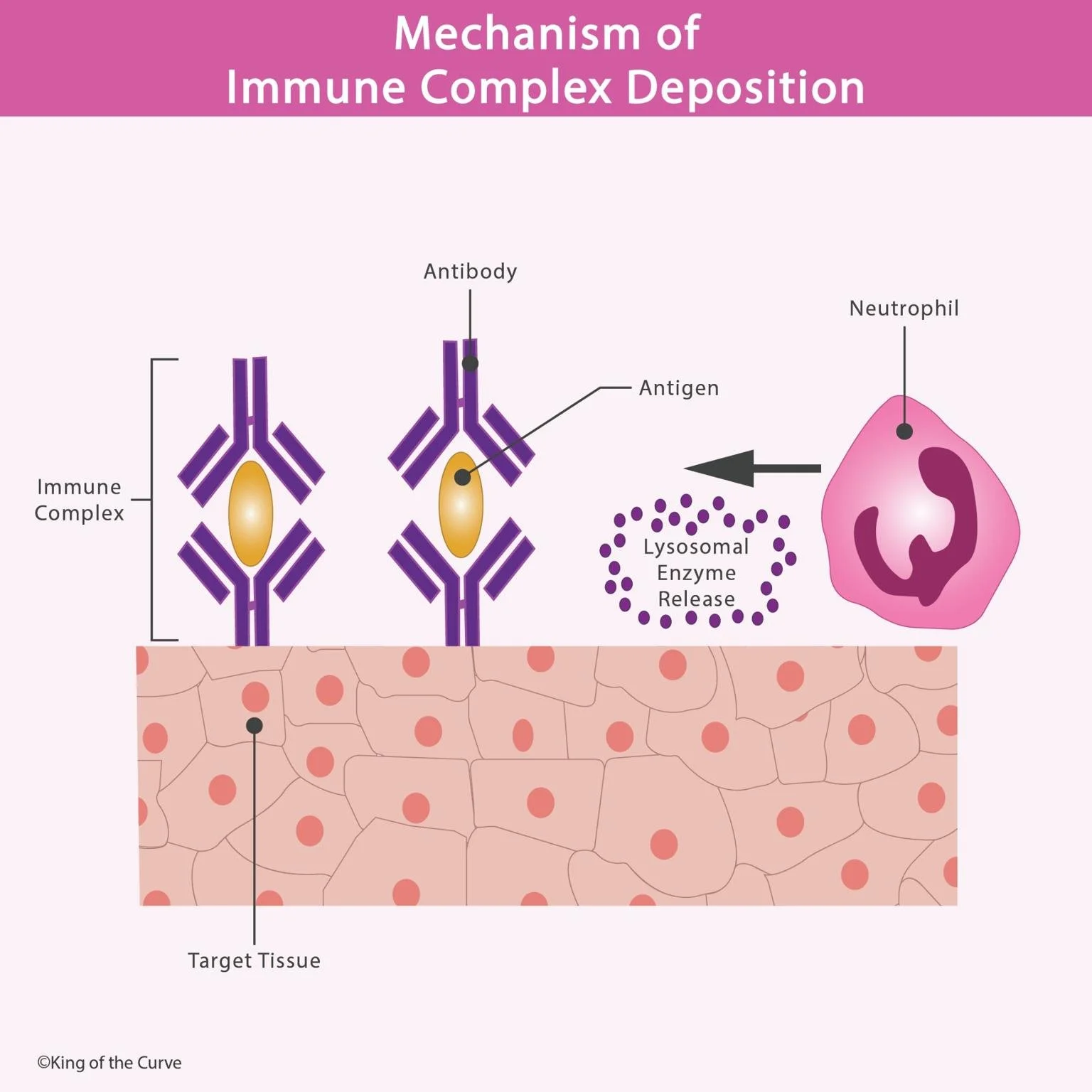
The immune system protects the body from pathogens through antibodies that bind to antigens, forming immune complexes. Normally, these complexes are cleared by phagocytic cells such as macrophages. However, when excessive complexes form or clearance mechanisms fail, they deposit in tissues — triggering inflammation and tissue injury.
This process, known as immune complex deposition, is central to Type III hypersensitivity reactions, which are implicated in diseases like systemic lupus erythematosus (SLE), rheumatoid arthritis, and post-streptococcal glomerulonephritis.
⚙️ Step-by-Step Mechanism
Formation of Immune Complexes:
Antibodies (typically IgG or IgM) bind to soluble antigens, creating circulating immune complexes.Deposition in Tissues:
These complexes become lodged in blood vessel walls, kidneys, joints, or lungs — especially in areas of high pressure or filtration.Complement Activation:
Deposited immune complexes trigger the complement cascade, releasing inflammatory mediators like C3a and C5a that attract neutrophils.Inflammatory Response:
Neutrophils migrate to the site and release lysosomal enzymes and reactive oxygen species, leading to local tissue injury and necrosis.
📊 Table: Key Concepts of Immune Complex Deposition
| Stage | Process | Result |
|---|---|---|
| 1. Immune Complex Formation | Antigen binds with antibody in circulation | Forms soluble immune complexes |
| 2. Deposition | Complexes lodge in tissues with high filtration pressure | Triggers complement activation |
| 3. Complement Activation | Release of C3a and C5a | Recruits inflammatory cells |
| 4. Neutrophil Involvement | Neutrophils release lysosomal enzymes | Tissue inflammation and damage |
🧩 Clinical Correlation
Immune complex deposition is often observed in autoimmune conditions where antibodies mistakenly target self-antigens. The resulting inflammation damages the very tissues the immune system is meant to protect. Understanding this mechanism is crucial for diagnosing and managing diseases like lupus nephritis or serum sickness.
🧠 Expanded Insight
The severity of tissue injury depends on several factors — including the size and charge of immune complexes, the efficiency of complement clearance, and genetic susceptibility. For example, small complexes tend to remain in circulation longer and deposit more easily in vessel walls. Additionally, deficiencies in complement proteins (like C2 or C4) increase the risk of immune complex–mediated diseases.
Histological findings often reveal fibrinoid necrosis, leukocytoclastic vasculitis, and granular deposits on immunofluorescence, distinguishing immune complex diseases from other inflammatory conditions.
💡 Therapeutic Perspective & Final Takeaway
Treatment aims to reduce immune complex formation and inflammation. Corticosteroids, immunosuppressants, and plasmapheresis are commonly used to decrease immune activity and remove circulating complexes. Research into biologics targeting complement components offers promising new avenues for therapy.
Ultimately, immune complex deposition highlights the fine line between defense and self-destruction — emphasizing how precision in immune regulation is vital for maintaining health.
Frequently Asked Questions (FAQs)
-
Aim for 4-6 focused hours, ensuring you incorporate breaks to avoid burnout.
-
Practice mindfulness techniques, take practice exams under realistic conditions, and maintain a balanced lifestyle.
-
Set short-term goals, seek support from mentors, and reward yourself for small achievements.
-
Regular exercise improves focus, reduces stress, and enhances overall mental clarity.
-
KOTC offers personalized learning tools, gamification features, and adaptive question banks to help students stay on track without burnout.