Bell’s Palsy: Causes, Symptoms, and Treatment
Bell’s palsy is a sudden-onset facial nerve paralysis that affects one side of the face, leading to asymmetry, difficulty closing the eye, and loss of facial expressions. It is often linked to viral reactivation and can mimic more severe neurological conditions like stroke, making early diagnosis and treatment crucial.
This guide explains the etiology, clinical presentation, diagnosis, and management of Bell’s palsy, making it a high-yield topic for medical students preparing for USMLE, NCLEX, and clinical practice.
Etiology: What Causes Bell’s Palsy?
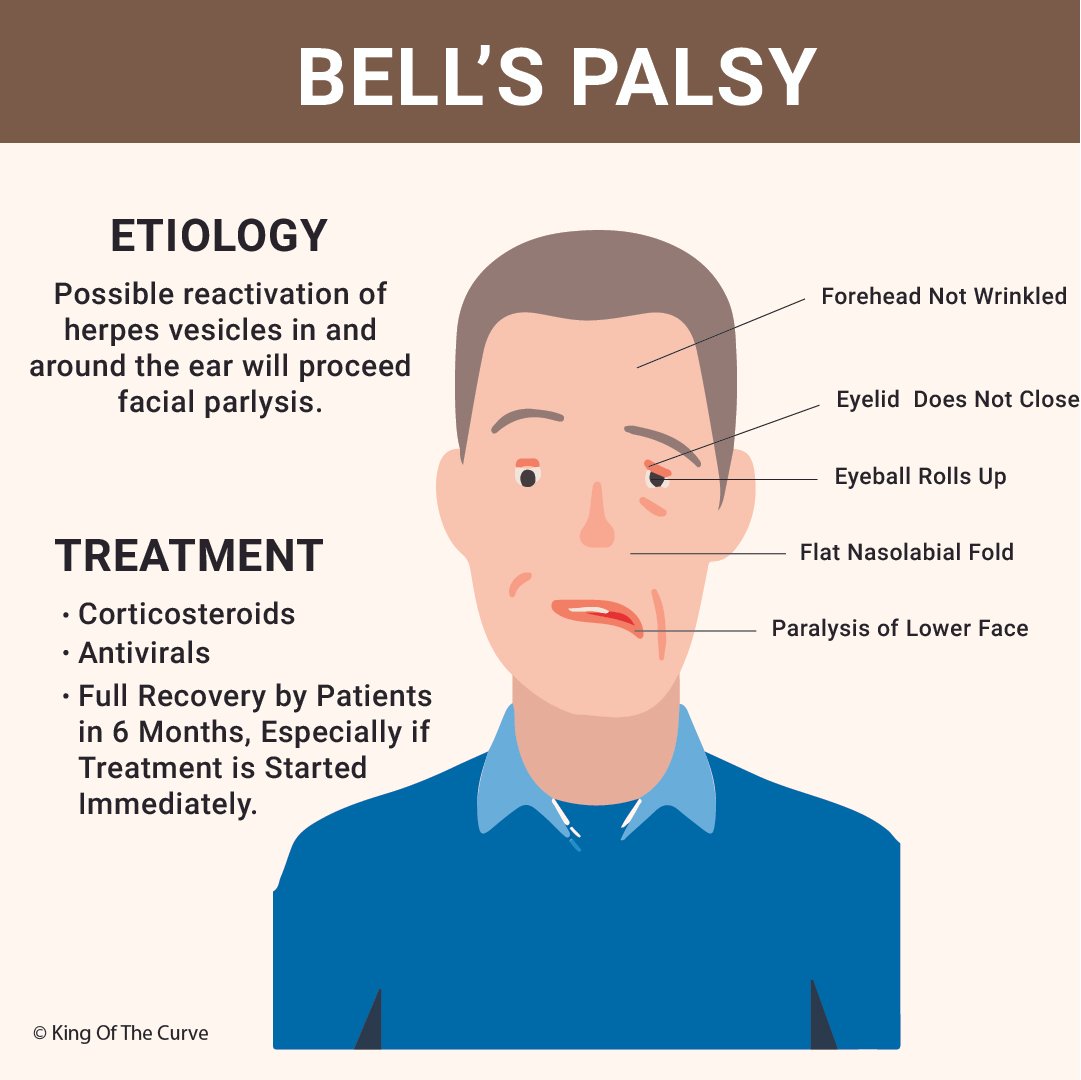
Bell’s palsy results from inflammation and compression of the facial nerve (cranial nerve VII), often due to viral reactivation.
🔹 Most common cause: Reactivation of Herpes Simplex Virus (HSV-1)
🔹 Other possible triggers:
Varicella-Zoster Virus (Ramsay Hunt Syndrome)
Epstein-Barr Virus (EBV)
Cytomegalovirus (CMV)
Lyme Disease
Autoimmune reactions
Cold exposure or stress
Key Pathophysiology:
Viral reactivation → Inflammation of CN VII → Facial nerve edema and compression
Leads to weakness or paralysis of facial muscles
Clinical Presentation: How to Recognize Bell’s Palsy?
✅ Rapid onset (<72 hours) of unilateral facial weakness
✅ Forehead involvement (unable to wrinkle forehead)
✅ Eyelid does not close → Risk of corneal ulceration
✅ Eyeball rolls upward (Bell’s phenomenon)
✅ Flattened nasolabial fold
✅ Drooping mouth and difficulty speaking or eating
✅ Altered taste sensation (anterior 2/3 of tongue)
🚨 Bell’s Palsy vs. Stroke: How to Differentiate?
Bell’s Palsy: Entire half of the face affected, including the forehead
Stroke: Forehead is spared due to bilateral cortical innervation of upper face
Diagnosis: Clinical and Investigations
Bell’s palsy is a clinical diagnosis, but some tests help rule out other causes:
🩺 Clinical exam: Evaluate facial muscle strength and symmetry
🩻 MRI/CT scan: If stroke, tumor, or multiple sclerosis is suspected
🩸 Serology: Lyme disease testing (if endemic area), viral markers
🛑 Electromyography (EMG): To assess nerve damage severity
Treatment and Management
🔹 Corticosteroids (Prednisone 60-80 mg/day for 7-10 days) → Best if started within 72 hours
🔹 Antiviral therapy (Acyclovir or Valacyclovir) → If viral etiology suspected
🔹 Eye care (Lubricating drops, eye patch at night) → Prevent corneal damage
🔹 Physical therapy and facial exercises → Prevent muscle stiffness
🔹 Surgical decompression (rarely needed) → If severe nerve compression
✅ Prognosis:
85% of patients recover fully within 6 months, especially with early treatment
Poor prognosis: Age >60, complete paralysis at onset, Ramsay Hunt syndrome
USMLE/NCLEX Exam Tip
📌 A 35-year-old male presents with sudden-onset left-sided facial weakness. He cannot close his left eye, has drooping of the mouth, and loss of taste sensation on the left side. There is no limb weakness or speech difficulty.
💡 Diagnosis: Bell’s Palsy
👉 Next Step: Start Prednisone within 72 hours
Conclusion
Bell’s palsy is a common and treatable cause of facial paralysis, often due to HSV-1 reactivation. Early corticosteroid therapy, eye care, and physical therapy ensure faster recovery and better outcomes.
📌 Want more high-yield medical content? Check out King of the Curve for detailed visuals and practice questions!